Heart failure is a chronic clinical syndrome in which the heart is unable to pump blood effectively to meet the body’s metabolic demands. It is typically the end stage of various cardiovascular diseases and is associated with high morbidity, mortality, and healthcare costs.
According to the Heart Failure Policy Network, approximately 90,000 people in Ireland live with heart failure. The prevalence increases significantly with age, affecting over 10% of individuals aged 70 and older. In the UK, the condition affects over 1 million people, accounting for 5% of all emergency hospital admissions.
Heart failure can result from multiple conditions that damage or overwork the heart muscle, including:
In particular, hypertension and diabetes are major contributors. Among patients with heart failure, up to 40–60% have a history of hypertension, and 20–40% have diabetes.
Heart failure is commonly divided into two major subtypes:
Diagnosis relies on a combination of clinical symptoms (e.g., breathlessness, fatigue, oedema), biomarkers (BNP or NT-proBNP), imaging (primarily echocardiography), and medical history.
Despite these diagnostic tools, underdiagnosis remains a significant issue, especially in patients with HFpEF, where symptoms overlap with other chronic conditions such as COPD or general frailty.
The 5-year mortality rate for heart failure remains high, estimated at 45–60%, depending on severity and comorbidities. Hospitalisation is frequent: in Ireland, heart failure accounts for over 20,000 inpatient bed days annually.
Readmission rates are also substantial. In the UK, 20–25% of patients hospitalised for heart failure are readmitted within 30 days.
Management of heart failure includes lifestyle changes, pharmacological treatment, and in some cases, device therapy or surgical intervention.
Pharmacological options include:
Non-pharmacological strategies include fluid restriction, sodium control, daily weight monitoring, and patient education to recognise early signs of decompensation.
In many cases, heart failure is only diagnosed during an acute hospital admission. Primary care settings often miss early indicators due to:
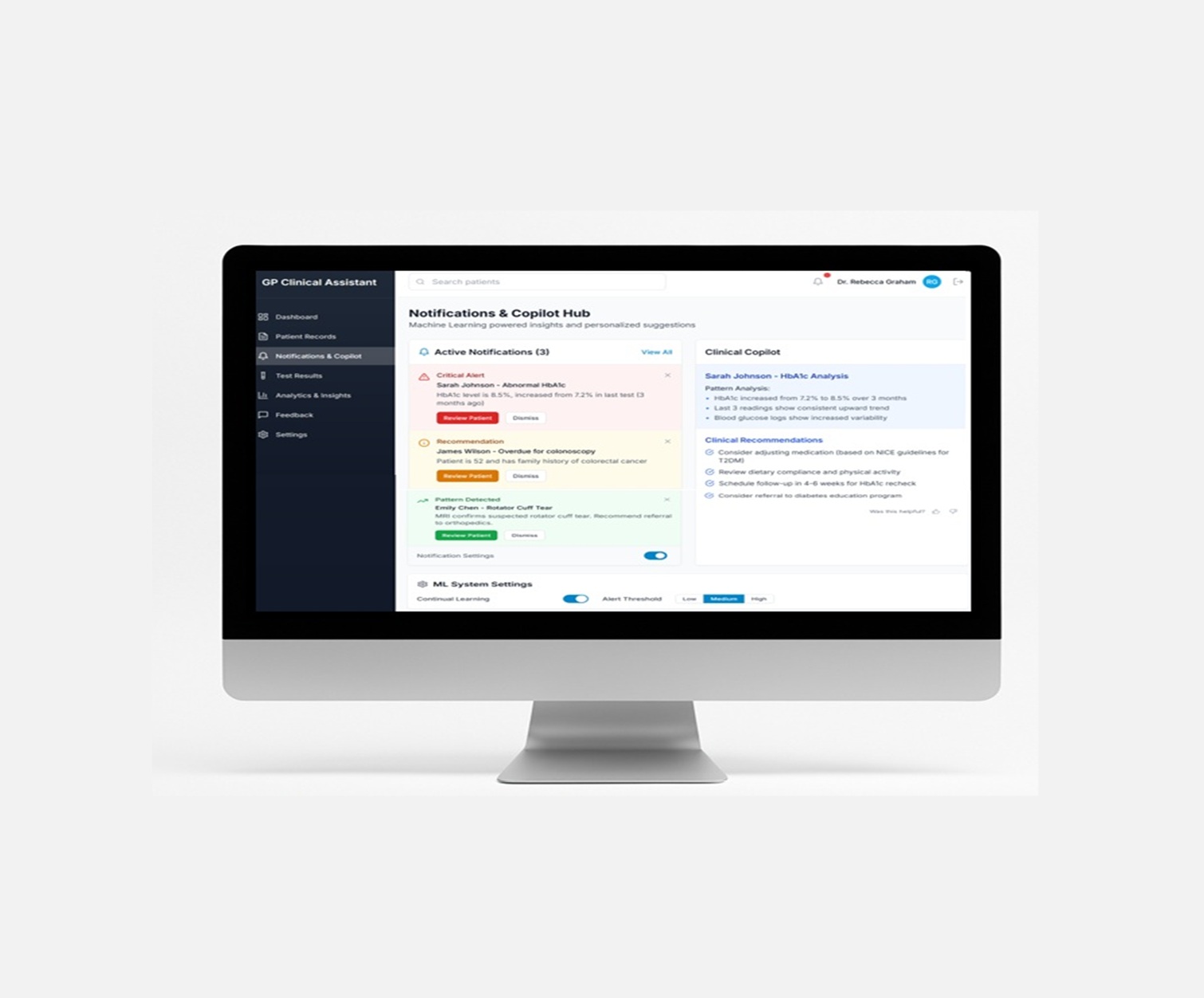
Improving early detection in primary care could reduce admissions and improve outcomes. Tools that aggregate clinical history, identify trends in weight gain or symptom reporting, and prompt testing could be beneficial.
Heart failure is common, complex, and costly. It is often detected late, and outcomes are poor once hospitalisation occurs. Structured monitoring, especially in high-risk populations, combined with prompt diagnostic testing, offers a route to earlier diagnosis and improved patient care.
Improved data integration, proactive case finding, and decision support in primary care may help bridge current gaps in detection and management.
Sign up to get early access and see how it works — before we go live.

“Follow the copywriting outline on every page. We made it ourselves, it’s battle-tested and you can be confident that it converts.”
Main benefit
Briefly expand on how this benefit will help your customers.
Second benefit
Briefly expand on how this benefit will help your customers.
Third benefit
Briefly expand on how this benefit will help your customers.